Olga Krzyzaniak won the 3RCC 3Rs Day Poster Prize 2025
 Free Download here
Free Download hereIllustrative poster by our PhD Student Frida Nilsson for FELASA 2025
 Download here
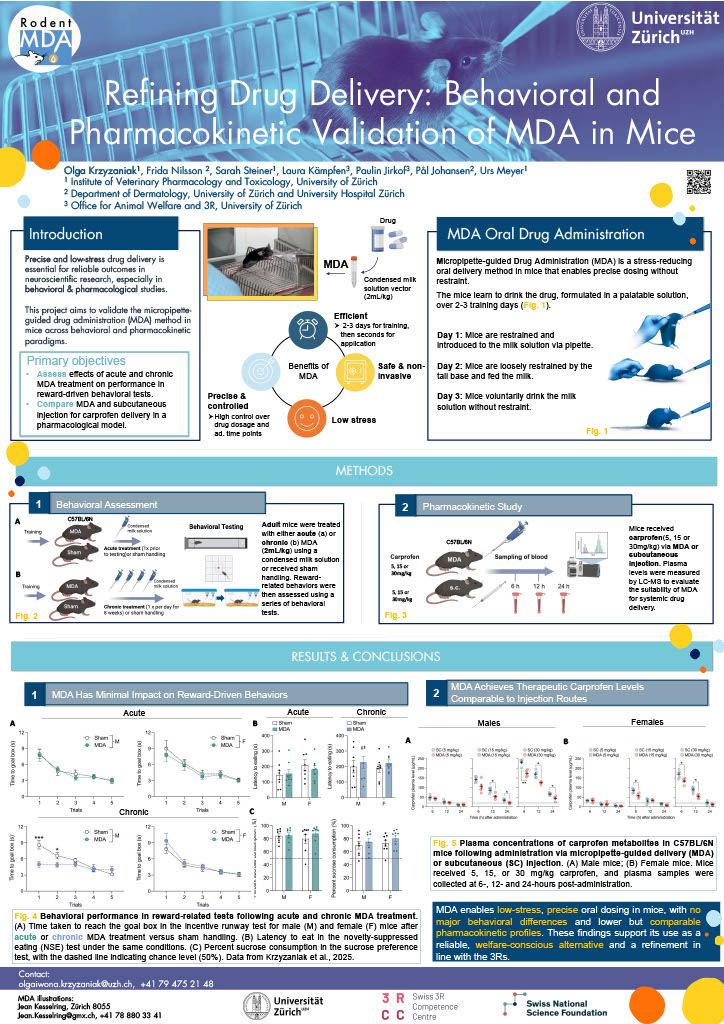
Download hereWhat is Rodent MDA and what is our research project actually about? This poster presents our NRP79 funded research project "Minimizing Stress and Harm for Laboratory Rodents in Oral Drug Treatments Using the Micropipette-guided Drug Administration (MDA)". Feel free to download and read through it.
 Download Poster
Download PosterThis is a constantly growing collection of recently published literature about the MDA method in rodents both from our team as well as from fellow researchers.
In this great compendium, the authors mention MDA and our work by Scarborough et al. 2020 in Chapter 5.4. Have a look!
Orogastric gavage is a common technique used to administer test articles to rodents with risks ranging from increased stress to death of the animal. In this study, we propose a novel technique to administer treatments to mice for voluntary consump tion through a plastic gavage needle: gavage-needle voluntary consumption (GVC) with a sweetened condensed milk carrier. GVC was successful at orally dosing mice in 95.0% (n = 459) of 483 total GVC opportunities. BALB/c mice (n = 61 [27 males/34 females] for analysis) were randomized into 8 intervention-treatment groups with 2 treatment allocations. Mice habituated to the GVC technique in less than 5 d and continued to consume the condensed milk with or without capromorelin for a 3-d treatment period that commenced after receiving their assigned interventions. The GVC technique allowed for efficient transition to orogastric gavage when the treatment was not consumed in 3.8% (n = 7) of 183 GVC attempts in the treatment period, thereby ensuring that every mouse received its treatment. The proportion of mice that consumed their treatments voluntarily was not affected by the intervention the mice received prior to the treatment period but was affected by the addition of the treatment article capromorelin. It is recommended to consider the GVC technique as a replacement and refinement to oral gavage when orogastric administration of treatments to mice is required.
To provide an alternative to oral gavage for per os treatments in laboratory mice, we have recently developed and introduced the micropipette-guided drug administration (MDA) method. This procedure is based on the presentation of a palatable solution consisting of sweetened condensed milk diluted with water, encouraging voluntary consumption of the vehicle and drug formulations. In this study, we compared the MDA method in male and female C57BL/6N and BALB/c mice, two inbred strains widely used in basic and preclinical research. Administering a diluted condensed milk solution daily over a period of 30 days, we observed that male C57BL/6N mice reached the fully voluntary drinking stage within five days or less, requiring the least amount of time to drink from the micropipette. Compared with males, female C57BL/6N mice showed increased consumption times during the initial administration period, yet they all managed to reach a fully voluntary stage within seven days or less. By contrast, BALB/c mice in general, and female BALB/c mice in particular, consistently required more time to consume the diluted condensed milk solution, whether administered voluntarily (no restraint) or semi-voluntarily (with mild tail restraint). Notably, a substantial portion of BALB/c mice (12.5% of males and 62.5% of females) failed to achieve fully voluntary consumption by MDA, despite their ability and willingness to drink the condensed milk solution when using a mild tail restraint. Taken together, the present study identified significant strain and sex differences in the MDA method as applied to laboratory mice.
Oral gavage is the standard method for acute or chronic per os treatments in laboratory rodents. It can, however, induce significant stress responses and compromise the welfare of animals. To mitigate these concerns, we recently introduced the micropipette-guided drug administration (MDA) method, which utilizes a palatable vehicle (diluted sweetened condensed milk) for voluntary ingestion of drug solutions. While MDA minimizes stress and potential injury, the sugar content of the vehicle raises concerns about its possible influence on reward-related behaviors.. This study examined whether acute or chronic exposure to the MDA vehicle affects the performance of male and female C57BL/6 mice in three behavioral tests that are commonly used to assess reward-related functions, namely the novelty-suppressed eating, sucrose preference, and incentive runway tests. Compared to corresponding sham handling, neither acute nor chronic exposure to the MDA vehicle affected novelty-suppressed eating or sucrose preference in either sex. However, chronic but not acute exposure to the MDA vehicle influenced the animals’ performance in the incentive runway test, with a significant effect observed in male mice specifically. This sex-dependent outcome suggests that male mice may be more susceptible to changes in reward-seeking behavior after chronic exposure to the MDA vehicle. In conclusion, our findings support the suitability of the MDA method for studies utilizing the novelty-suppressed eating and sucrose preference tests, while highlighting the need for careful consideration when assessing reward-seeking behavior in male mice using the incentive runway test.
Oral gavage is a widely used method to infect mice with Cryptosporidium parvum (CP), the most common animal model of infection. Cryptosporidium spp. are worldwide distributed, gastrointestinal parasites that mainly cause diarrhea in humans and neonatal ruminants. CP is transmitted via the fecal–oral route, usually through contaminated water. In rodent models of Cryptosporidium infection, oral gavage is used as the route of infection. This method, while effective, induces a generalized stress response and requires specific skills and experience. Our aim was to replace oral gavage by a refined method using a mixture palatable to mice, where oocysts could be mixed in. A peanut butter gelatin mix (PBG) containing CP oocysts was developed and used for voluntary oral infection of mice. We were able to confirm CP infections in young interferon-gamma knock out mice by detecting oocyst shedding in feces, demonstrating that the PBG method successfully produced infections similar to those obtain through oral gavage, and could be used for other pathogens or as a method to deliver experimental therapeutics or other substances.
Voluntary oral drug administration using sweet substances promotes rodents’ therapeutic compliance while reducing stress induced by forced drug administration. We aimed to test whether rats would willingly eat strawberry jam or condensed milk from a syringe, and which one they would prefer. Our results show that rats prefer condensed milk, demonstrating its potential as a vehicle for the voluntary oral administration of drugs in experimental protocols.
A glucose tolerance test (GTT) is routinely used to assess glucose homeostasis in clinical settings and in preclinical research studies using rodent models. The procedure assesses the ability of the body to clear glucose from the blood in a defined time after a bolus dose. In the human clinical setting, glucose is ingested via voluntary consumption of a clucose-sweetened drink. Typically, in the rodent GTT oral gavage (gavage-oGTT) or (more commonly) intraperitoneal injection (IPGTT) are used to administer the glucose bolus. Although used less frequently, likely due to investigator technical and experience barriers, the former is the more physiologically relevant as it integrates the gastrointestinal tract (GI), including release of key incretin hormones. However, orally gavaging glucose in the GTT is also not without its limitations: gavaging glucose straight into the stomach bypasses potentially critical early glucose-sensing via the mouth (cephalic phase) and associated physiological responses. Furthermore, gavaging is stressful on mice, and this by itself can increase blood glucose levels. We have developed and validated a refined protocol for mouse oral GTT which uses a voluntary oral glucose dosing method, micropipette-guided drug administration (MDA), without the need for water deprivation. This approach is simple and non-invasive. It is less stressful for the mice, as evidenced by lower circulating corticosterone levels 10 minutes after glucose-dosing compared to oral gavage. This is significant for animal and investigator welfare, and importantly minimising the confounding effect of stress on mouse glucose homeostasis. Using a randomised cross-over design, we have validated the MDA approach in the oGTT against oral gavage in male and female C57BL/6J and C57BL/6N mice. We show the ability of this method to detect changes in glucose tolerance in diet- nduced obese animals. Compared to oral gavage there was lower inter-animal variation in the MDA-oGTT. In addition to being more representative of the human procedure, the MDA-oGTT is easy and has lower barriers to adoption than the gavage oGTT as it is non-invasive and requires no specialist equipment or operator training. The MDA-oGTT a more clinically representative, accessible, and refined replacement for the gavage-oGTT for mouse metabolic phenotyping, which is simple yet overcomes significant deficiencies in the current standard experimental approaches.
Oral gavage (OG) with the use of a cannula attached to a syringe is one of the most common methods used to deliver precise dosing of compounds to the stomach of research animals. Unfortunately, this method comes with difficulties for both the operator and the research animal. Studies have shown that OG may lead to complications, including esophagitis, perforation of the esophagus, and inadvertent tracheal drug administration. In addition, OG is associated with increased plasma and fecal corticosterone levels (due to stress), altered blood pressure, and increased heart rate, which could negatively influence or bias study results. A previously developed alternative method termed micropipette-guided drug administration (MDA) incentivizes the animal to consume treatments readily in a minimally invasive manner. Herein, we present examples of the use of the MDA technique with treatments reconstituted in different vehicles and demonstrate effective delivery of the varied treatments to multiple different mouse strains. We further demonstrate that MDA is a technique that decreases the timing and invasiveness of drug administration and does not affect the gut microbiome composition as assessed by quantitative analysis of core gut microbial species. Overall, MDA may offer a less stressful and effective alternative to OG.
Drug administration in preclinical rodent models is essential for research and the development of novel therapies. Compassionate administration methods have been developed, but these are mostly incompatible with water-insoluble drugs such as tamoxifen or do not allow for precise timing or dosing of the drugs. For more than two decades, tamoxifen has been administered by oral gavage or injection to CreERT2–loxP gene-modified mouse models to spatiotemporally control gene expression, with the numbers of such inducible models steadily increasing in recent years. Animal-friendly procedures for accurately administering tamoxifen or other water-insoluble drugs would, therefore, have an important impact on animal welfare. On the basis of a previously published micropipette feeding protocol, we developed palatable formulations to encourage voluntary consumption of tamoxifen. We evaluated the acceptance of the new formulations by mice during training and treatment and assessed the efficacy of tamoxifen-mediated induction of CreERT2–loxP-dependent reporter genes. Both sweetened milk and syrup-based formulations encouraged mice to consume tamoxifen voluntarily, but only sweetened milk formulations were statistically noninferior to oral gavage or intraperitoneal injections in inducing CreERT2-mediated gene expression. Serum concentrations of tamoxifen metabolites, quantified using an in-house-developed cell assay, confirmed the lower efficacy of syrup- as compared to sweetened milk-based formulations. We found dosing with a micropipette to be more accurate than oral gavage or injection, with the added advantage that the method requires little training for the experimenter. The new palatable solutions encourage voluntary consumption of tamoxifen without loss of efficacy compared to oral gavage or injections and thus represent a refined administration method.
Oral vaccines are gaining attention for their ease of administration and ability to activate mucosal immune responses. However, preclinical studies using this route often require the use of gavage, which has limitations. In this comment, we briefly discuss the challenges associated with gavage as a technique for studying oral vaccine administration in preclinical models and explore alternative methods.
Background: In preclinical studies resorting to rodents, the effects of prolonged oral intake of active substances are difficult to evaluate. Indeed, to get closer to clinical reality, oral gavage (OG) is frequently used but the repetition of administrations induces risks of lesions of the digestive tract, and stress for animals which can compromise the quality of the results. New method: This study describes the development of a non-invasive oral administration method in male Sprague Dawley rats, as a safe alternative of OG, more faithful to clinical reality and limiting biases in pharmacokinetics and/or pharmacodynamics interpretation. Micropipette-guided Drug Administration (MDA) is based on the administration by micropipette of a sufficiently palatable vehicle for the animals to voluntarily take its contents. Results: MDA was not demonstrated as less stressful than OG. A pharmacokinetics equivalence between MDA and OG was demonstrated for pregabalin administration but not for aripiprazole. Despite the use of a sweet vehicle, the MDA method does not result in weight gain or significant elevation of blood glucose and fructosamines level. Regarding the time needed to administrate the solution, the MDA method is significantly faster than OG. Comparison with existing method(s): Contrastingly to procedures using food or water, this method allows for a rigorous control of the time and dose administered and is delivered in discrete administration windows which is therefore closer to the clinical reality. This method appears particularly suitable for pharmacological evaluation of hydrophilic compounds. Conclusions: The MDA procedure represents a respectful and adapted pharmacological administration method to study the effects of chronic oral administration in rats.
The designer receptor exclusively activated by designer drugs (DREADD) system is one of the most widely used chemogenetic techniques to modulate the activity of cell populations in the brains of behaving animals. DREADDs are activated by acute or chronic administration of their ligand, clozapine-N-oxide (CNO). There is, however, a current lack of a non-invasive CNO administration technique that can control for drug timing and dosing without inducing substantial distress for the animals. Here, we evaluated whether the recently developed micropipette-guided drug administration (MDA) method, which has been used as a non-invasive and minimally stressful alternative to oral gavages, may be applied to administer CNO orally to activate DREADDs in a dosing- and timing-controlled manner. Unlike standard intraperitoneal injections, administration of vehicle substances via MDA did not elevate plasma levels of the major stress hormone, corticosterone, and did not attenuate exploratory activity in the open field test. At the same time, however, administration of CNO via MDA or intraperitoneally was equally efficient in activating hM3DGq-expressing neurons in the medial prefrontal cortex, as evident by time-dependent increases in mRNA levels of neuronal immediate early genes (cFos, Arc and Zif268) and cFos-immunoreactive neurons. Compared to vehicle given via MDA, oral administration of CNO via MDA was also found to potently increase locomotor activity in mice that express hM3DGq in prefrontal neurons. Taken together, our study confirms the effectiveness of CNO given orally via MDA and provides a novel method for non-stressful, yet well controllable CNO treatments in mouse DREADD systems.
Pharmacological treatments in laboratory rodents remain a cornerstone of preclinical psychopharmacological research and drug development. There are numerous ways in which acute or chronic pharmacological treatments can be implemented, with each method having certain advantages and drawbacks. Here, we describe and validate a novel treatment method in mice, which we refer to as the micropipette-guided drug administration (MDA) procedure. This administration method is based on a sweetened condensed milk solution as a vehicle for pharmacological substances, which motivates the animals to consume vehicle and/or drug solutions voluntarily in the presence of the experimenter. In a proof-of-concept study, we show that the pharmacokinetic profiles of the atypical antipsychotic drug, risperidone, were similar whether administered via the MDA procedure or via the conventional oral gavage method. Unlike the latter, however, MDA did not induce the stress hormone, corticosterone. Furthermore, we assessed the suitability and validity of the MDA method in a mouse model of maternal immune activation, which is frequently used as a model of immune-mediated neurodevelopmental disorders. Using this model, we found that chronic treatment (>4 weeks, once per day) with risperidone via MDA led to a dose-dependent mitigation of MIA-induced social interaction deficits and amphetamine hypersensitivity. Taken together, the MDA procedure described herein represents a novel pharmacological administration method for per os treatments in mice that is easy to implement, cost effective, non-invasive, and less stressful for the animals than conventional oral gavage methods.

In colaboration with the French 3R Center FC3R we now have a French translation of our Rodent MDA SOP
Download here